Data from prespecified co-primary endpoints showed the mean LDL-C reduction from baseline at weeks 22 and 24 was 54.5 percent for Repatha compared to 16.7 percent for ezetimibe (p<0.001). At week 24, LDL-C reduction was 52.8 percent for Repatha compared to 16.7 percent for ezetimibe (p<0.001). At baseline, the mean LDL-C level was 219.9 mg/dL for all patients entering the active-controlled part of the trial. Muscle-related side effects were reported in 20.7 percent of Repatha patients and 28.8 percent of ezetimibe patients. In patients treated with ezetimibe, active study drug was stopped for muscle symptoms in 6.8 percent of patients, compared to 0.7 percent of patients treated with Repatha.
"Statin-associated muscle symptoms represent a major unresolved challenge in the care of patients with cardiovascular disease," said
The GAUSS-3 study built upon knowledge gained from the GAUSS-1 and GAUSS-2 studies, which used patient-reported incidence of statin-related side effects. GAUSS-3 employed a rigorous active statin rechallenge in patients with history of intolerance to two or more statins to determine a patient population that experienced MRSE on statin therapy but not on placebo. Despite the short, 10-week rechallenge, more than 40 percent of patients rechallenged with atorvastatin developed intolerable muscle side effects to atorvastatin and not placebo.
"By employing a unique crossover design, these study results provide insights into our understanding of statin intolerance, which can be difficult to define from patient-reported symptoms alone," said co-lead author
In the GAUSS-3 trial there were no new safety findings. The most common adverse events that occurred in greater than 5 percent of patients in the Repatha group were myalgia (13.8 percent Repatha; 21.9 percent ezetimibe), nasopharyngitis (9.7 percent Repatha; 2.7 percent ezetimibe), muscle spasms (9.0 percent Repatha; 6.8 percent ezetimibe), arthralgia (9.0 percent Repatha; 1.4 percent ezetimibe), pain in extremity (9.0 percent Repatha; 1.4 percent ezetimibe), fatigue (8.3 percent Repatha; 6.8 percent ezetimibe), headache (6.9 percent Repatha; 9.6 percent ezetimibe) and back pain (6.9 percent Repatha; 8.2 percent ezetimibe).
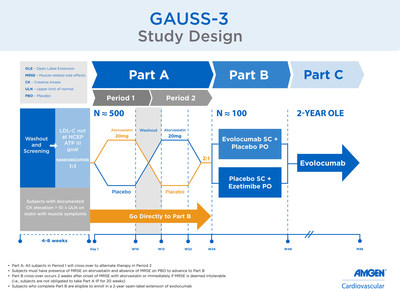
GAUSS-3 Study Design
GAUSS-3 (Goal Achievement After Utilizing an Anti-PCSK9 Antibody in Statin Intolerant Subjects-3) is a Phase 3, multicenter, randomized, double-blind, placebo-controlled statin rechallenge trial designed to evaluate the safety, tolerability and efficacy of Repatha in 491 patients with high cholesterol who could not tolerate statins due to MRSE.
The study was divided into three parts (A, B, C):
The co-primary endpoints were the mean percent reductions from baseline in LDL-C at weeks 22 and 24 and the percent reduction from baseline in LDL-C at week 24 in Part B. Secondary efficacy endpoints included means at weeks 22 and 24 and at week 24 for the following: change from baseline in LDL-C; LDL-C response <70 mg/dL; change from baseline in total cholesterol (TC); change from baseline in non-high-density lipoprotein cholesterol (non-HDL-C), apolipoprotein B (ApoB), TC/HDL-C ratio, ApoB/apolipoprotein A1 (ApoA1) ratio, lipoprotein(a), triglycerides, HDL-C and very low-density lipoprotein cholesterol (VLDL-C).
About Repatha® (evolocumab)
Repatha® (evolocumab) is a human monoclonal antibody that inhibits proprotein convertase subtilisin/kexin type 9 (PCSK9). Repatha binds to PCSK9 and inhibits circulating PCSK9 from binding to the low-density lipoprotein (LDL) receptor (LDLR), preventing PCSK9-mediated LDLR degradation and permitting LDLR to recycle back to the liver cell surface. By inhibiting the binding of PCSK9 to LDLR, Repatha increases the number of LDLRs available to clear LDL from the blood, thereby lowering LDL-C levels.1
GLAGOV, the intravascular ultrasound study, is underway to determine the effect of Repatha on coronary atherosclerosis in approximately 950 patients undergoing cardiac catheterization to test the hypothesis of robust LDL-C reduction leading to a reduction or a change in the build-up of plaque in the arteries. Results from the GLAGOV study are expected in the second half of 2016.
The FOURIER outcomes trial is designed to evaluate whether treatment with Repatha in combination with statin therapy, compared to placebo plus statin therapy, reduces the risk of cardiovascular events in patients with high cholesterol and clinically evident cardiovascular disease, and completed patient enrollment in June 2015. Top-line results from the approximately 27,500-patient event-driven FOURIER study are anticipated in the second half of 2016.
Repatha is approved in
Important U.S. Product Information
Repatha® is indicated as an adjunct to diet and:
The effect of Repatha® on cardiovascular morbidity and mortality has not been determined.
The safety and effectiveness of Repatha® have not been established in pediatric patients with HoFH who are younger than 13 years old.
The safety and effectiveness of Repatha® have not been established in pediatric patients with primary hyperlipidemia or HeFH.
Important Safety Information
Contraindication: Repatha® is contraindicated in patients with a history of a serious hypersensitivity reaction to Repatha®.
Allergic reactions: Hypersensitivity reactions (e.g. rash, urticaria) have been reported in patients treated with Repatha®, including some that led to discontinuation of therapy. If signs or symptoms of serious allergic reactions occur, discontinue treatment with Repatha®, treat according to the standard of care, and monitor until signs and symptoms resolve.
Adverse reactions: The most common adverse reactions (>5% of Repatha®-treated patients and more common than placebo) were: nasopharyngitis, upper respiratory tract infection, influenza, back pain, and injection site reactions.
In a 52-week trial, adverse reactions led to discontinuation of treatment in 2.2% of Repatha®-treated patients and 1% of placebo-treated patients. The most common adverse reaction that led to Repatha® treatment discontinuation and occurred at a rate greater than placebo was myalgia (0.3% versus 0% for Repatha® and placebo, respectively).
Adverse reactions from a pool of the 52-week trial and seven 12-week trials:
Local injection site reactions occurred in 3.2% and 3.0% of Repatha®-treated and placebo-treated patients, respectively. The most common injection site reactions were erythema, pain, and bruising. The proportions of patients who discontinued treatment due to local injection site reactions in Repatha®-treated patients and placebo-treated patients were 0.1% and 0%, respectively.
Allergic reactions occurred in 5.1% and 4.7% of Repatha®-treated and placebo-treated patients, respectively. The most common allergic reactions were rash (1.0% versus 0.5% for Repatha® and placebo, respectively), eczema (0.4% versus 0.2%), erythema (0.4% versus 0.2%), and urticaria (0.4% versus 0.1%).
Neurocognitive events were reported in less than or equal to 0.2% in Repatha®-treated and placebo-treated patients.
In a pool of placebo- and active-controlled trials, as well as open-label extension studies that followed them, a total of 1,988 patients treated with Repatha® had at least one LDL-C value <25 mg/dL. Changes to background lipid-altering therapy were not made in response to low LDL-C values, and Repatha® dosing was not modified or interrupted on this basis. Although adverse consequences of very low LDL-C were not identified in these trials, the long-term effects of very low levels of LDL-C induced by Repatha® are unknown.
Musculoskeletal adverse reactions were reported in 14.3% of Repatha®-treated patients and 12.8% of placebo-treated patients. The most common adverse reactions that occurred at a rate greater than placebo were back pain (3.2% versus 2.9% for Repatha® and placebo, respectively), arthralgia (2.3% versus 2.2%), and myalgia (2.0% versus 1.8%).
Homozygous Familial Hypercholesterolemia (HoFH): In 49 patients with homozygous familial hypercholesterolemia studied in a 12-week, double-blind, randomized, placebo-controlled trial, 33 patients received 420 mg of Repatha® subcutaneously once monthly. The adverse reactions that occurred in at least 2 (6.1%) Repatha®-treated patients and more frequently than in placebo-treated patients, included upper respiratory tract infection (9.1% versus 6.3%), influenza (9.1% versus 0%), gastroenteritis (6.1% versus 0%), and nasopharyngitis (6.1% versus 0%).
Immunogenicity: Repatha® is a human monoclonal antibody. As with all therapeutic proteins, there is a potential for immunogenicity with Repatha®.
Please contact Amgen Medinfo at 800-77-AMGEN (800-772-6436) or 844-REPATHA (844-737-2842) regarding Repatha® availability or find more information, including full Prescribing Information, at www.amgen.com and www.Repatha.com.
About Amgen Cardiovascular
Building on more than three decades of experience in developing biotechnology medicines for patients with serious illnesses,
About
For more information, visit www.amgen.com and follow us on www.twitter.com/amgen.
Amgen Forward-Looking Statements
This news release contains forward-looking statements that are based on the current expectations and beliefs of
No forward-looking statement can be guaranteed and actual results may differ materially from those we project. Discovery or identification of new product candidates or development of new indications for existing products cannot be guaranteed and movement from concept to product is uncertain; consequently, there can be no guarantee that any particular product candidate or development of a new indication for an existing product will be successful and become a commercial product. Further, preclinical results do not guarantee safe and effective performance of product candidates in humans. The complexity of the human body cannot be perfectly, or sometimes, even adequately modeled by computer or cell culture systems or animal models. The length of time that it takes for us to complete clinical trials and obtain regulatory approval for product marketing has in the past varied and we expect similar variability in the future. Even when clinical trials are successful, regulatory authorities may question the sufficiency for approval of the trial endpoints we have selected. We develop product candidates internally and through licensing collaborations, partnerships and joint ventures. Product candidates that are derived from relationships may be subject to disputes between the parties or may prove to be not as effective or as safe as we may have believed at the time of entering into such relationship. Also, we or others could identify safety, side effects or manufacturing problems with our products after they are on the market.
Our results may be affected by our ability to successfully market both new and existing products domestically and internationally, clinical and regulatory developments involving current and future products, sales growth of recently launched products, competition from other products including biosimilars, difficulties or delays in manufacturing our products and global economic conditions. In addition, sales of our products are affected by pricing pressure, political and public scrutiny and reimbursement policies imposed by third-party payers, including governments, private insurance plans and managed care providers and may be affected by regulatory, clinical and guideline developments and domestic and international trends toward managed care and healthcare cost containment. Furthermore, our research, testing, pricing, marketing and other operations are subject to extensive regulation by domestic and foreign government regulatory authorities. We or others could identify safety, side effects or manufacturing problems with our products after they are on the market. Our business may be impacted by government investigations, litigation and product liability claims. In addition, our business may be impacted by the adoption of new tax legislation or exposure to additional tax liabilities. If we fail to meet the compliance obligations in the corporate integrity agreement between us and the U.S. government, we could become subject to significant sanctions. Further, while we routinely obtain patents for our products and technology, the protection offered by our patents and patent applications may be challenged, invalidated or circumvented by our competitors, or we may fail to prevail in present and future intellectual property litigation. We perform a substantial amount of our commercial manufacturing activities at a few key facilities and also depend on third parties for a portion of our manufacturing activities, and limits on supply may constrain sales of certain of our current products and product candidate development. In addition, we compete with other companies with respect to many of our marketed products as well as for the discovery and development of new products. Further, some raw materials, medical devices and component parts for our products are supplied by sole third-party suppliers. The discovery of significant problems with a product similar to one of our products that implicate an entire class of products could have a material adverse effect on sales of the affected products and on our business and results of operations. Our efforts to acquire other companies or products and to integrate the operations of companies we have acquired may not be successful. We may not be able to access the capital and credit markets on terms that are favorable to us, or at all. We are increasingly dependent on information technology systems, infrastructure and data security. Our stock price is volatile and may be affected by a number of events. Our business performance could affect or limit the ability of our Board of Directors to declare a dividend or our ability to pay a dividend or repurchase our common stock.
CONTACT:
References

Photo - http://photos.prnewswire.com/prnh/20160401/350600
Logo - http://photos.prnewswire.com/prnh/20081015/AMGENLOGO
To view the original version on PR Newswire, visit:http://www.prnewswire.com/news-releases/positive-efficacy-and-tolerability-study-of-repatha-evolocumab-in-statin-intolerant-patients-published-in-journal-of-the-american-medical-association-300245197.html
SOURCE